Precise Diagnosis Using Modern Technology
Accurate diagnosis is the foundation of excellent medical care. Many gynecologic and hormonal conditions cannot be diagnosed by symptoms alone—they require targeted imaging and laboratory testing to clearly identify the cause and guide the right treatment.
According to the National Institutes of Health (NIH) and the CDC, delayed or incomplete diagnostic testing is one of the most common reasons women experience years of untreated pain, delayed cancer diagnoses, repeated ineffective treatments, fertility delays, and worsening chronic conditions.
Modern diagnostic technology allows us to see, measure, and understand what is happening inside the body—early, safely, and precisely.
Pelvic Ultrasound
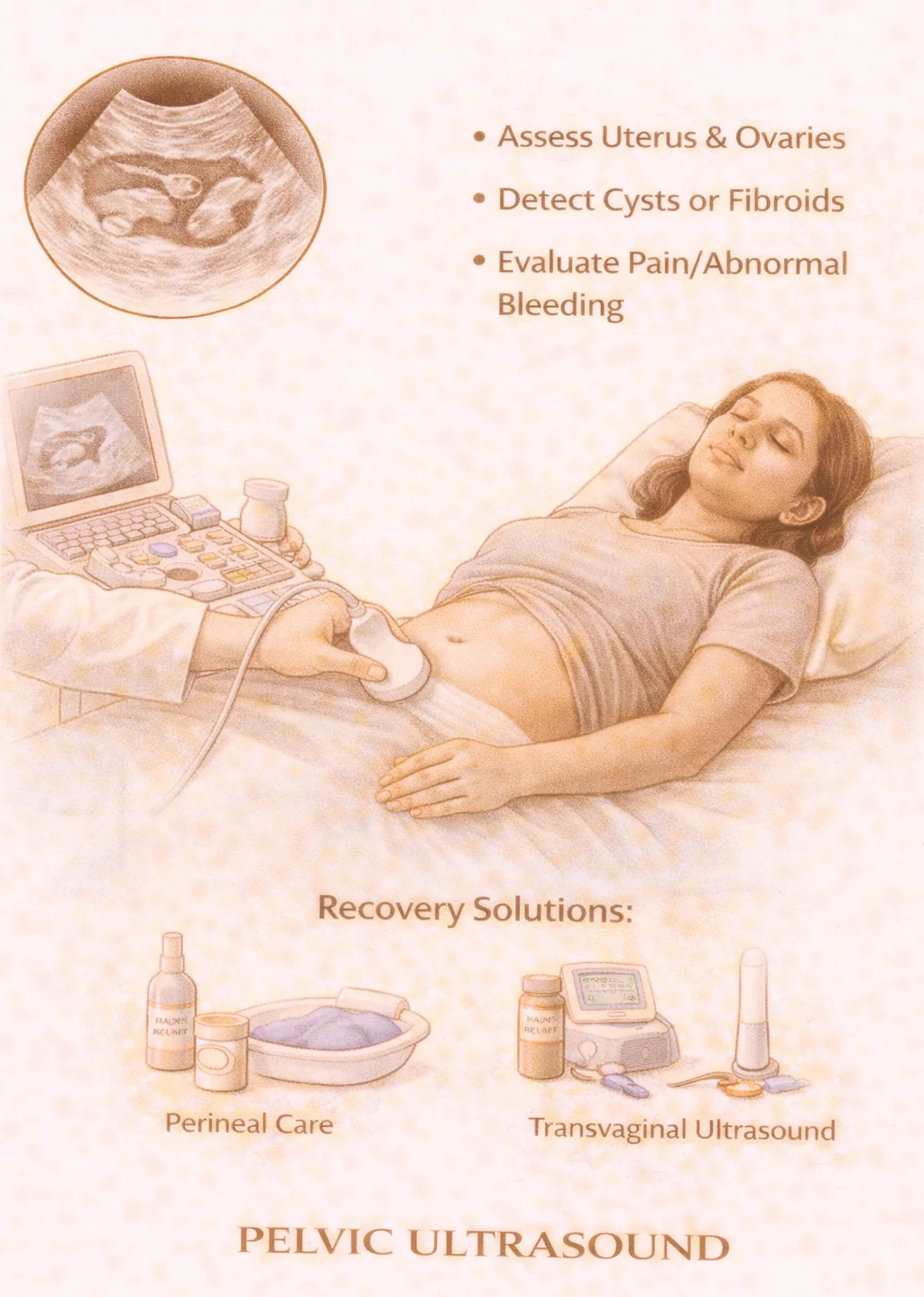
What it is: A non-invasive imaging test that uses sound waves to view the uterus, ovaries, and pelvic structures through the abdomen.
Why it matters: According to ACOG and the NIH, pelvic ultrasound is often the first-line imaging tool for evaluating abnormal uterine bleeding, pelvic pain, fibroids, ovarian cysts, pelvic masses, and pregnancy location. It helps determine uterine size and shape, presence of fibroids or polyps, ovarian cyst characteristics, and fluid or pelvic abnormalities.
When neglected: Without imaging, conditions such as large fibroids, complex cysts, or early pregnancy complications may remain undetected until symptoms become severe.
Transvaginal Ultrasound
What it is: A specialized ultrasound performed with a small internal probe to give high-resolution, close-up views of the uterus and ovaries.
Why it matters: According to ACOG, transvaginal ultrasound provides far greater detail than abdominal ultrasound alone. It is essential for early pregnancy evaluation, identifying endometrial abnormalities, detecting small ovarian cysts, fibroid mapping, and evaluating infertility.
When neglected: Relying only on abdominal imaging can miss early endometrial disease, subtle cysts, or early pregnancy complications such as ectopic pregnancy.
Saline Infusion Sonography (SIS)
What it is: An advanced ultrasound technique in which sterile saline is gently placed into the uterus to clearly outline the uterine cavity.
Why it matters: According to ACOG and NIH, SIS is the most accurate non-surgical test for detecting uterine polyps, submucosal fibroids, scar tissue (Asherman's syndrome), and structural causes of infertility or bleeding. It provides near-hysteroscopy-level detail without surgery.
When neglected: Many women with persistent bleeding are treated repeatedly with hormones when a structural cause (like a polyp or fibroid) is actually responsible.
Hormonal & Endocrine Testing

What it is: Blood testing to evaluate key hormones that regulate menstrual cycles, ovulation, fertility, metabolism, mood, energy, weight, and menopause symptoms. Common tests include thyroid hormones, estrogen & progesterone, FSH & LH, testosterone, prolactin, and insulin and glucose markers.
Why it matters: According to the CDC and NIH, thyroid disease affects 1 in 8 women, and PCOS affects 1 in 10 women. Hormonal imbalance is a leading cause of irregular cycles, infertility, weight changes, hair and skin changes, fatigue, and mood shifts.
When neglected: Without proper hormone testing, women are often told their symptoms are "just stress" while a treatable endocrine imbalance continues unchecked.
Comprehensive STD Panels
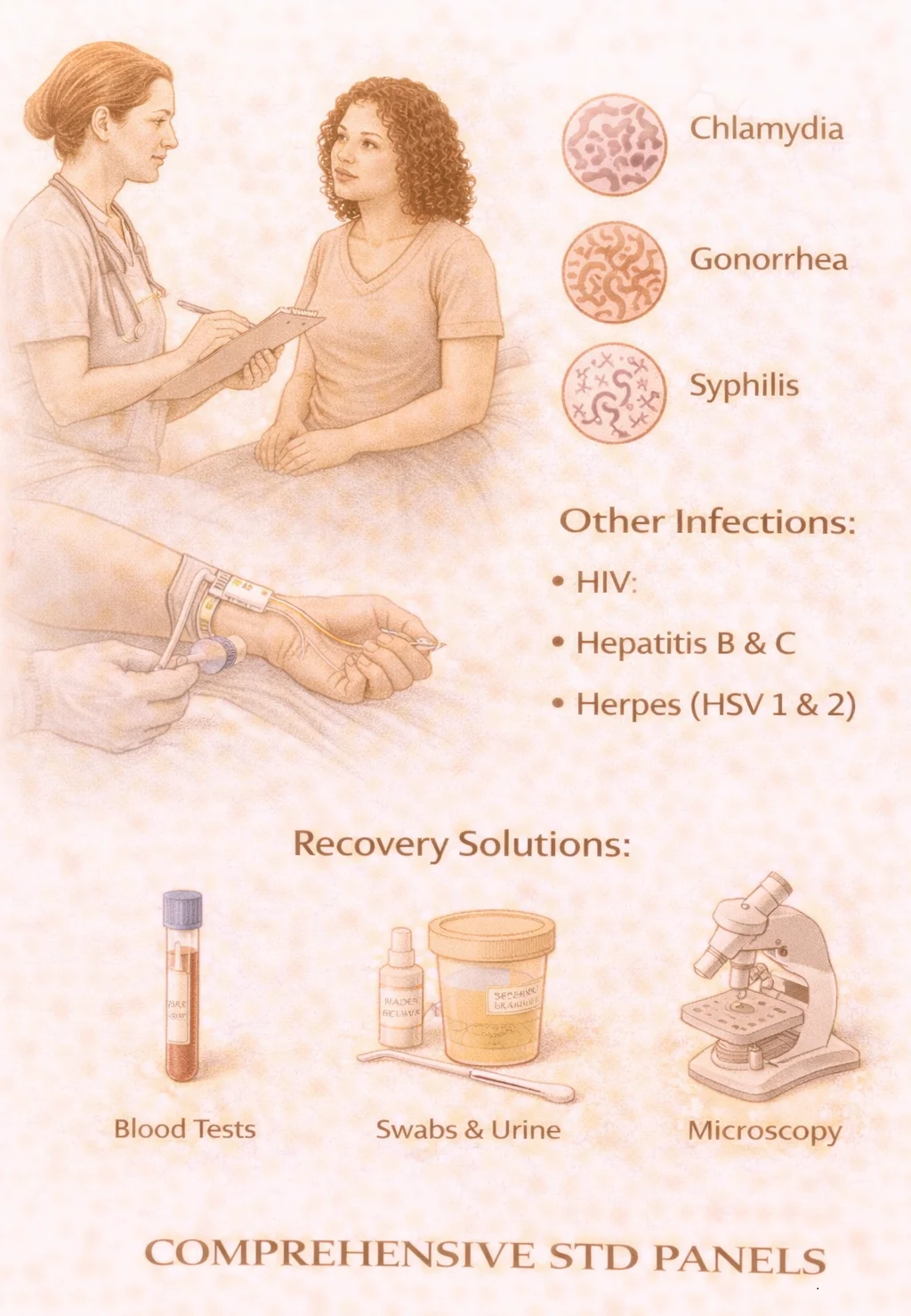
What they include: Accurate laboratory testing for chlamydia, gonorrhea, syphilis, trichomonas, HIV, hepatitis B & C, and HPV (when indicated).
Why they matter: According to the CDC, over 2 million STIs are diagnosed each year in the U.S. Many STIs in women cause no immediate symptoms. Untreated infections are a major cause of infertility, chronic pelvic pain, ectopic pregnancy, and pregnancy complications.
When neglected: Silent infections can damage fertility before symptoms ever appear. Regular testing protects both your health and your partner's health.
Genetic & High-Risk Screening

What it is: Testing for inherited conditions that may affect cancer risk, pregnancy outcomes, or future children. This includes genetic carrier screening, hereditary cancer risk panels (when indicated), and family-history-guided testing.
Why it matters: According to ACOG and the CDC, about 1 in 100 couples carry genes that increase risk of serious inherited disease. Most people who are carriers have no symptoms and no family history. Genetic screening supports informed pregnancy planning, early cancer surveillance, preventive care strategies, and family risk protection.
When neglected: Genetic conditions are often discovered only after a child is affected or cancer develops—when prevention opportunities have already passed.
Diagnostic testing is not just about finding problems—it's about clarity, peace of mind, and empowering you with the information needed to make the best decisions for your health.

