Advanced Care for Complex Conditions
Need complex gynecology care in Northern Virginia?
Some gynecologic conditions go far beyond routine care. They are severe, persistent, recurrent, or anatomically complex—often affecting fertility, daily function, emotional health, and long-term outcomes. Many women with these conditions have already seen multiple providers, tried multiple treatments, and still struggle without clear answers.
According to the National Institutes of Health (NIH) and American College of Obstetricians and Gynecologists (ACOG), complex gynecologic disease is a leading cause of chronic pain, infertility, and repeat surgery in women. Delayed diagnosis and incomplete treatment significantly increase the risk of disease progression, surgical complications, and permanent organ damage.
High-risk and complex gynecology requires advanced imaging and diagnostic precision, subspecialty-trained surgical strategy, multidisciplinary coordination, and a patient-centered, long-term treatment plan. This level of care is about restoring function, protecting fertility when possible, and preventing repeat surgeries.
Severe Endometriosis
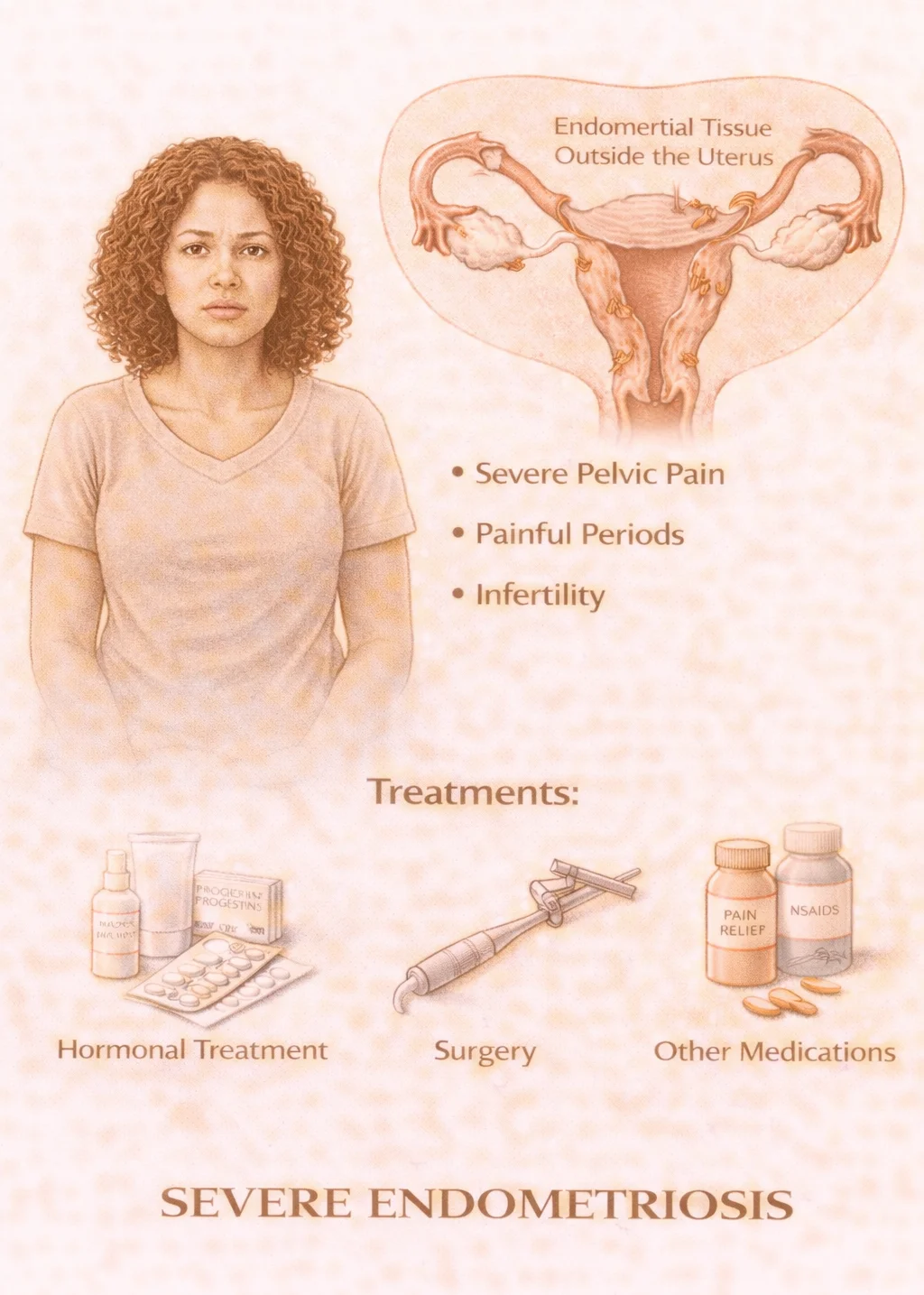
What it is: Advanced endometriosis involving deep infiltrating disease, bowel, bladder, or ureter involvement, dense pelvic scarring, severe pain, or infertility.
Why it matters: According to the CDC and NIH, endometriosis affects about 1 in 10 women and is present in up to 50% of women with infertility. Average diagnosis is delayed 7–10 years after symptom onset. Severe endometriosis can cause daily, disabling pain, pain with intercourse, bowel and urinary symptoms, recurrent ovarian cysts (endometriomas), and fertility damage.
When neglected: Untreated advanced endometriosis can lead to progressive organ scarring, bowel or ureter obstruction, permanent fertility impairment, and escalating surgical complexity with each procedure.
Large Fibroids

What it is: Uterine fibroids that are very large in size, numerous, deeply embedded in the uterine wall, distorting the uterine cavity, or compressing the bladder, bowel, or kidneys.
Why it matters: According to the NIH, up to 70–80% of women develop fibroids by age 50, and fibroids are the leading cause of hysterectomy in the U.S. Large fibroids are a major cause of severe bleeding, iron-deficiency anemia, pelvic pressure and pain, infertility, and pregnancy complications.
When neglected: Large fibroids can lead to transfusion-level anemia, kidney obstruction, recurrent pregnancy loss, emergency surgery, and loss of fertility options.
Chronic Pelvic Pain
What it is: Pelvic pain lasting more than 6 months, often with multiple overlapping causes.
Why it matters: According to the NIH, chronic pelvic pain affects nearly 15% of women and is one of the most common and complex pain syndromes in medicine. Causes may include endometriosis, pelvic floor dysfunction, adhesions, nerve entrapment, prior infections or surgery, and bladder or bowel disorders.
When neglected: Persistent pain may result in centralized nerve pain, opioid dependence, sexual dysfunction, depression and anxiety, job loss, and disability.
Recurrent Pregnancy Loss Evaluation

What it is: Advanced medical evaluation after two or more consecutive miscarriages.
Why it matters: According to the American Society for Reproductive Medicine (ASRM) and CDC, recurrent pregnancy loss affects about 1–2% of couples. Causes may include uterine structural abnormalities, fibroids or scar tissue, hormonal disorders, genetic factors, blood clotting conditions, and immune disorders. Evaluation may include advanced imaging, genetic testing, hormonal evaluation, and specialized laboratory studies.
When neglected: Without proper diagnosis, women may experience repeated unexplained losses, delayed fertility, emotional trauma and grief, and loss of confidence in future pregnancy success.
Colposcopy & Abnormal Pap Smear Management

What it is: Specialized magnified examination of the cervix used to evaluate abnormal Pap smears, positive high-risk HPV tests, visible cervical lesions, or unexplained abnormal bleeding.
Why it matters: According to the American Cancer Society and CDC, approximately 13,000 new cases of cervical cancer are diagnosed annually in the U.S., and most are preventable with proper screening and follow-up. Colposcopy allows precise identification and biopsy of precancerous changes (dysplasia or CIN) before they progress to invasive cancer. It is essential for triaging abnormal Pap smears, confirming HPV-related changes, guiding treatment decisions, and monitoring high-risk patients.
When neglected: Delayed or inadequate follow-up of abnormal Pap smears can allow cervical dysplasia to progress to invasive cancer, requiring far more aggressive treatment and threatening fertility and long-term survival.
Surgical Second Opinions
What it is: Independent expert review of recommended hysterectomy, fibroid surgery, endometriosis surgery, oophorectomy, or complex repeat surgeries.
Why it matters: According to the NIH and ACOG, a significant percentage of major gynecologic surgeries are later found to be unnecessary, incomplete, or unnecessarily aggressive. Second opinions help confirm whether surgery is truly needed, determine if minimally invasive options exist, preserve fertility when possible, and avoid irreversible procedures.
When neglected: Women may undergo preventable hysterectomy, incomplete endometriosis excision, repeat surgeries due to missed disease, and permanent fertility loss.
Complex Surgical Planning

What it is: Advanced pre-operative planning for difficult cases involving prior multiple abdominal surgeries, severe scar tissue, large fibroids, advanced endometriosis, combined bowel, bladder, or fertility surgery, and high-risk medical conditions.
Why it matters: According to ACOG and NIH, surgical complication rates rise significantly in repeat surgeries, dense adhesions, and deep pelvic disease. Proper planning dramatically reduces blood loss, organ injury, conversion to open surgery, and length of hospital stay. Complex planning often requires advanced imaging, multidisciplinary surgical coordination, fertility-preserving strategies, and robotic or advanced laparoscopic techniques.
When neglected: Without expert planning, women face higher risks of bowel or bladder injury, emergency open surgery, prolonged recovery, repeat operations, and permanent functional damage.
Complex gynecologic care is not just about treating disease—it's about restoring quality of life, protecting your future, and getting it right the first time.

