Whole-Woman Care Beyond the Exam Room
Excellent medical care does not stop at diagnosis or treatment—it continues through education, guidance, and long-term support. Many of the most powerful drivers of women's health outcomes are not found in a prescription alone, but in understanding, daily habits, emotional well-being, and informed decision-making.
According to the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH), health literacy strongly predicts health outcomes, medication adherence, and preventive screening behavior. Women who receive structured health education are more likely to follow through with treatment, detect warning symptoms earlier, and achieve better long-term disease control.
Patient education and support services ensure that you are informed, empowered, confident, and never navigating your health alone.
Personalized Health Education
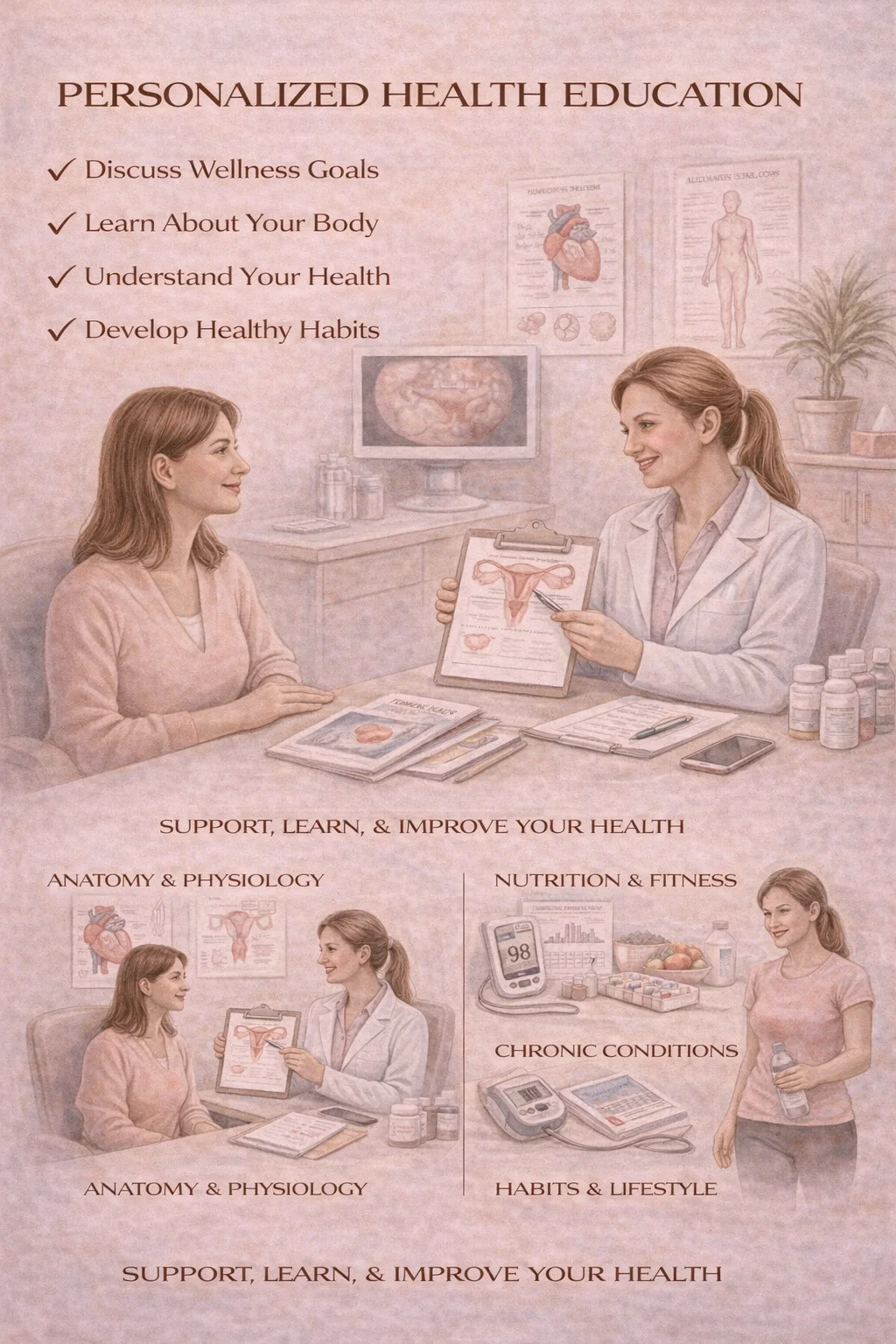
What it is: One-on-one education tailored specifically to your diagnosis, your life stage, your goals, and your cultural and personal values. This includes education on menstrual health, hormonal balance, chronic gynecologic conditions, fertility planning, menopause, and post-surgical recovery.
Why it matters: According to the NIH, patients who understand their condition and treatment plan experience higher treatment success rates, fewer emergency visits, and better long-term outcomes.
When neglected: Without personalized education, women often feel overwhelmed, confused, or fearful—leading to delayed care, poor adherence, and unnecessary complications.
Nutritional Counseling for Women
What it is: Targeted nutrition guidance based on hormonal health, metabolism, fertility goals, PCOS, endometriosis, menopause, and bone and heart health.
Why it matters: According to the CDC and NIH, nutrition is a major determinant of hormonal regulation, insulin sensitivity, fertility outcomes, bone density, and cardiovascular disease risk. Proper nutrition support can improve irregular cycles, inflammation, energy levels, weight stability, and pregnancy outcomes.
When neglected: Poor nutrition contributes to worsening PCOS, infertility, fatigue, osteoporosis, and cardiometabolic disease—often silently for years.
Stress & Lifestyle Guidance
What it is: Support for chronic stress, burnout, sleep disruption, work-life imbalance, and emotional load and caregiving strain.
Why it matters: According to the NIH and the American Heart Association, chronic stress in women is closely linked to hormonal dysregulation, menstrual irregularities, cardiovascular disease, anxiety and depression, and immune system suppression. Lifestyle guidance addresses sleep hygiene, physical activity, stress-reduction strategies, and sustainable daily routines.
When neglected: Unmanaged stress can worsen nearly every gynecologic condition—from infertility and pain disorders to menopause symptoms and chronic fatigue.
Fertility & Family Planning Education
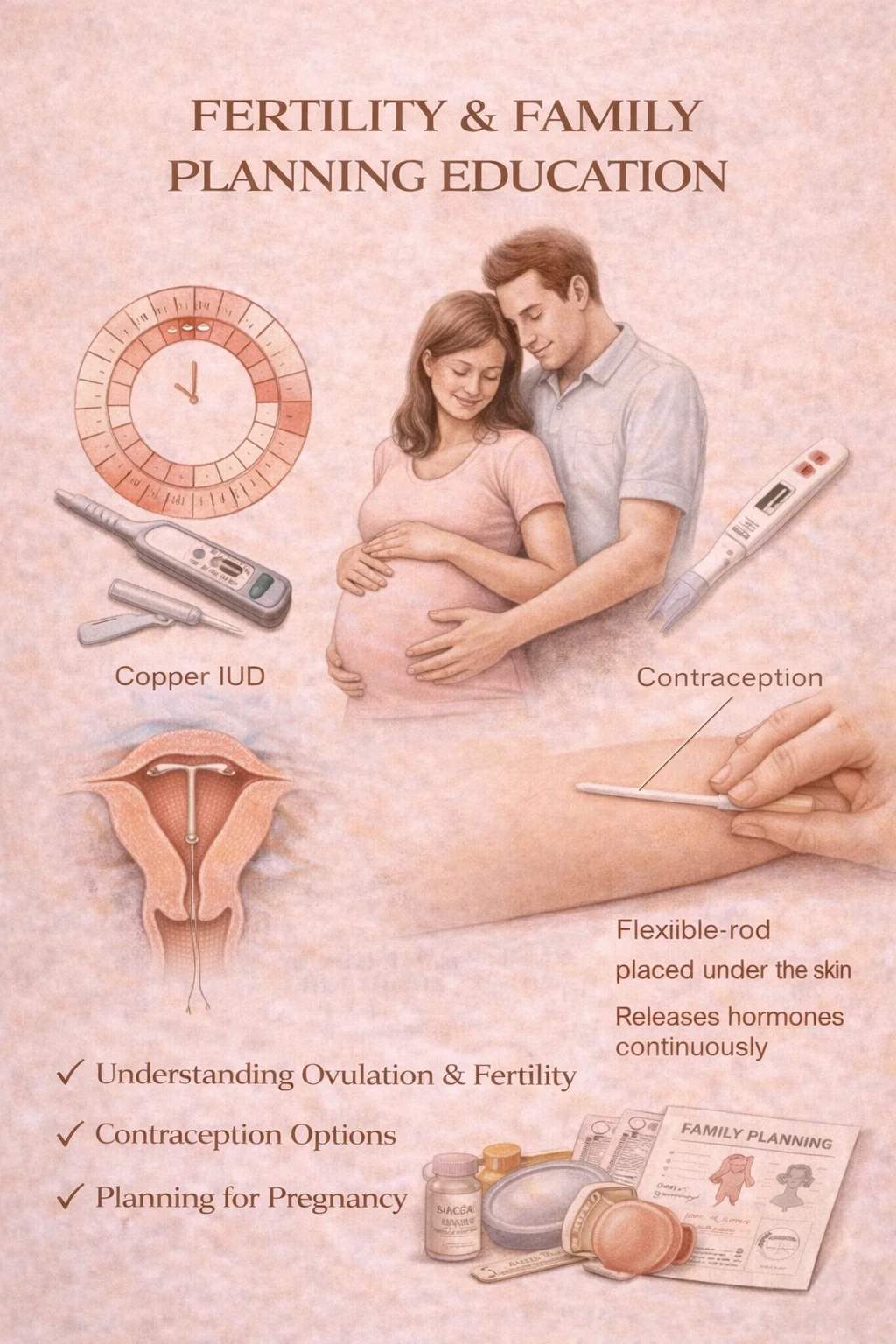
What it is: Education focused on fertility timing and realistic expectations, ovulation awareness, age-related fertility changes, contraceptive planning, and pregnancy optimization.
Why it matters: According to the NIH and American Society for Reproductive Medicine (ASRM), female fertility begins to decline in the early 30s and decline accelerates after age 35. Many women overestimate how long fertility remains robust. Education empowers women to plan proactively, preserve fertility when appropriate, and avoid preventable delays.
When neglected: Many women only discover fertility challenges after repeated unsuccessful attempts to conceive—when options may already be more limited.
Menopause Education Programs
What they are: Structured education around perimenopause, menopause, hormone therapy, non-hormonal management, bone health, heart health, brain health, and sexual wellness.
Why they matter: According to The Menopause Society and NIH, up to 80% of women experience disruptive menopause symptoms, and most women receive little to no formal education about menopause before symptoms begin. Education reduces fear, misinformation, unnecessary suffering, unsafe hormone use, and delayed treatment.
When neglected: Women often believe symptoms like brain fog, insomnia, weight gain, and sexual discomfort are "just aging" and miss the opportunity for effective treatment.
Surgical Education & Recovery Planning
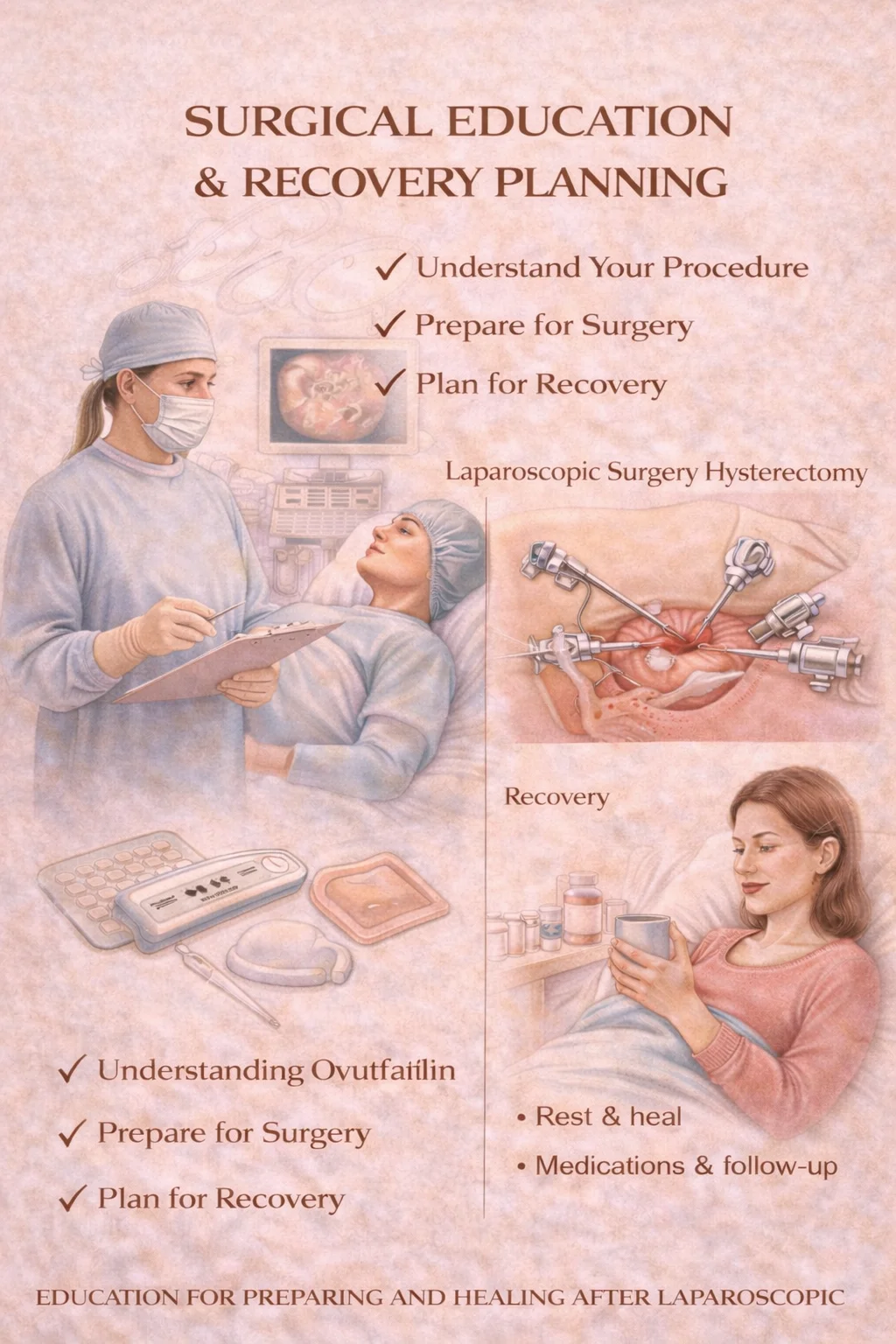
What it is: Comprehensive education before and after surgery, including what surgery involves, expected recovery timelines, pain control strategies, activity restrictions, warning signs, and emotional recovery support.
Why it matters: According to the CDC and NIH, structured surgical education reduces post-operative complications, improves pain control, decreases emergency room visits, and speeds safe return to work and daily life.
When neglected: Lack of education increases fear, confusion, delayed healing, and avoidable post-operative complications.
Aesthetic & Functional Gynecology Consultation
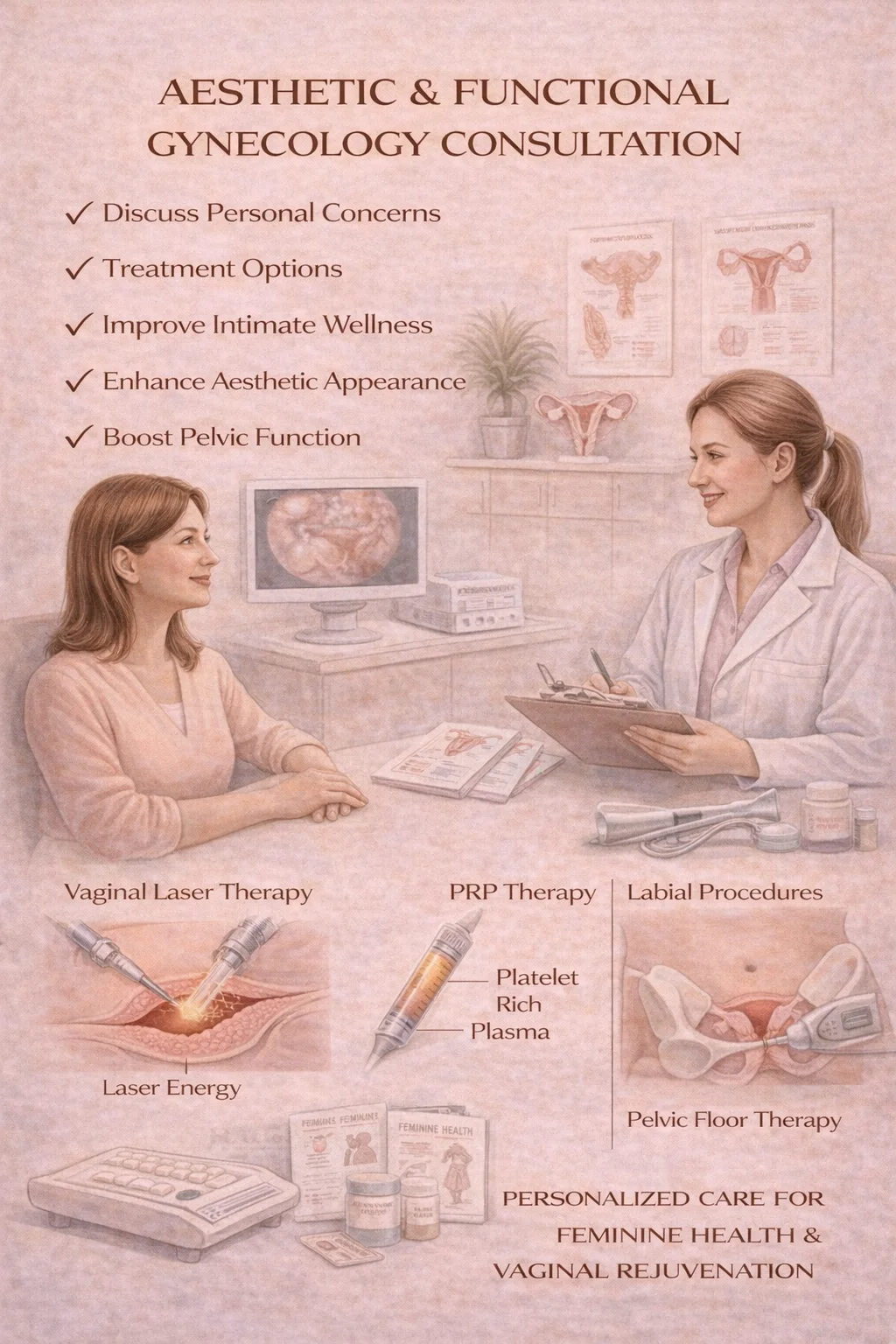
What it is: Confidential consultation for women seeking care related to vaginal comfort, tissue changes after childbirth or menopause, sexual confidence, and functional concerns affecting quality of life. These visits focus on medical evaluation, education on safe options, functional—not cosmetic-driven—outcomes, and individual goals and expectations.
Why it matters: According to the NIH and Menopause Society, hormonal changes and childbirth alter vaginal tissue, blood flow, elasticity, and nerve sensitivity. These changes can affect comfort, bladder control, and sexual function. Aesthetic & functional consultations allow women to ask questions safely, understand realistic options, and make informed, pressure-free decisions.
When neglected: Many women silently struggle with discomfort, loss of confidence, and relationship distress without ever realizing that safe, medical support exists.
Education is medicine. When women understand their bodies, they make better decisions, recover faster, and thrive longer.

