Continuity Before, During, and After Treatment
Surgery and medical treatment are not isolated events—they are part of a longer healing journey. True high-quality care does not end when the procedure is over. It continues through recovery, monitoring, prevention of complications, and long-term wellness.
According to the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH), a significant portion of post-surgical complications occur after hospital discharge. Long-term outcomes improve dramatically when patients receive structured pre-operative education, close post-operative follow-up, and ongoing chronic condition management.
Post-surgical and long-term care focus on safe recovery, pain control, return to daily function, prevention of future complications, and protection of long-term health and quality of life. This is where excellent outcomes become lasting outcomes.
Pre-Operative Counseling
What it is: A structured medical and educational visit before any planned procedure designed to prepare you physically, emotionally, and medically for surgery.
Why it matters: According to ACOG and the CDC, patients who receive structured pre-operative counseling experience fewer complications, less anxiety, faster recovery, and better pain control. Proper preparation reduces surgical site infections, medication errors, blood clot risk, and post-operative nausea and delays in recovery. Pre-op counseling includes review of imaging and diagnosis, surgical options and alternatives, fertility considerations, medication adjustments, anesthesia expectations, and recovery timeline and work restrictions.
When neglected: Without proper preparation, patients face higher anxiety, avoidable medication complications, delayed healing, and unexpected limitations after surgery.
Post-Operative Follow-Up
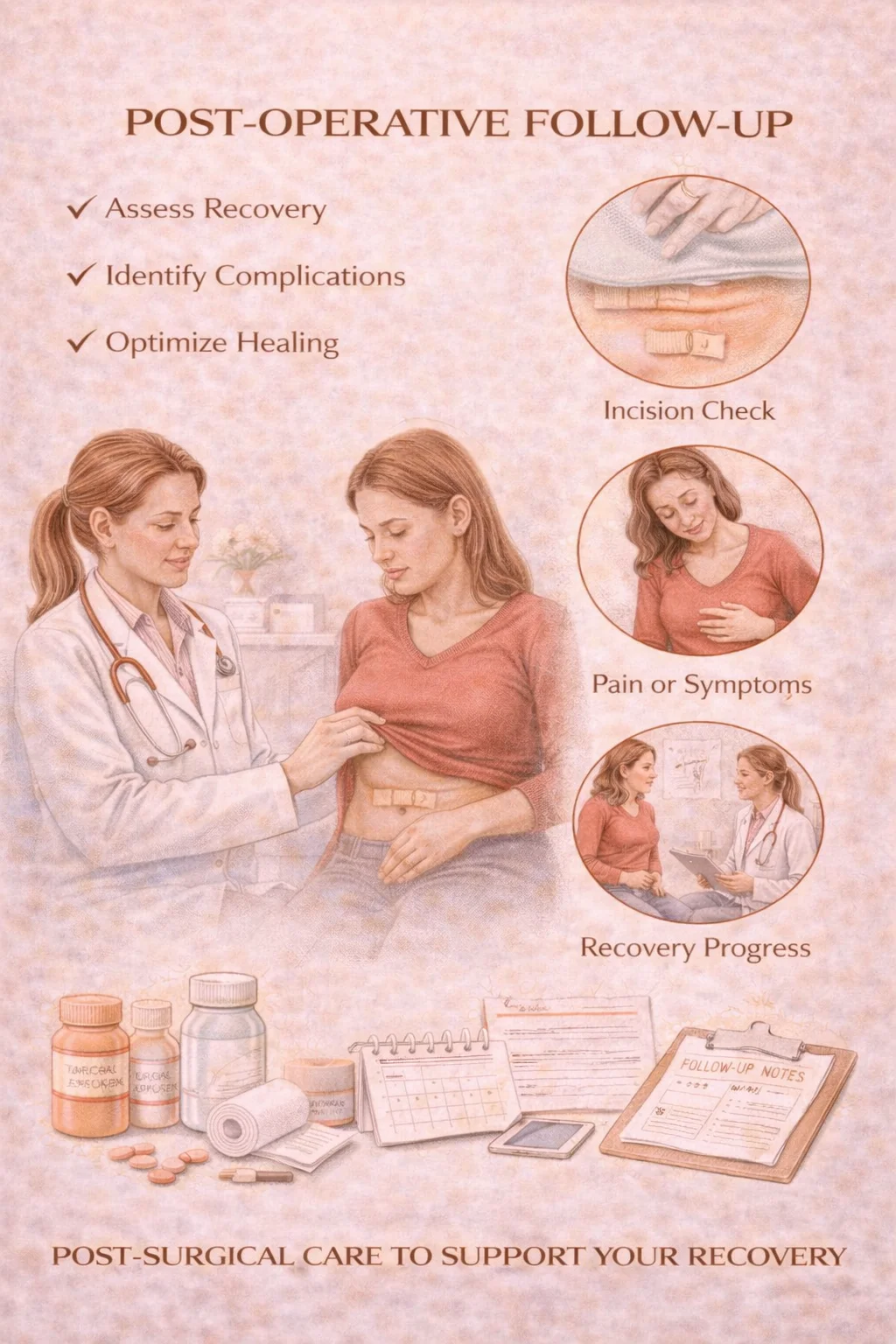
What it is: Scheduled, structured medical visits after surgery to assess healing, manage symptoms, and prevent complications.
Why it matters: According to the CDC, many post-surgical infections, blood clots, and wound complications develop after discharge. Early detection through follow-up reduces hospital readmissions, emergency room visits, and long-term surgical complications. Post-op care includes incision evaluation, pain and medication management, bladder and bowel recovery, activity and lifting guidance, infection and clot prevention, and emotional well-being support.
When neglected: Lack of follow-up increases risk of silent infections, unrecognized blood clots, poor wound healing, chronic post-surgical pain, and delayed return to work and normal life.
Long-Term Surgical Outcome Monitoring
What it is: Ongoing assessment of surgical success months to years after treatment.
Why it matters: According to the NIH and World Health Organization (WHO), some gynecologic conditions—such as endometriosis, fibroids, and pelvic adhesions—have recurrence risks over time. Long-term monitoring improves symptom control, re-intervention timing, fertility outcomes, and overall patient satisfaction. This monitoring includes symptom checks, imaging when indicated, hormone evaluations, menstrual and pain tracking, and fertility outcome review.
When neglected: Without long-term follow-up, recurrence may go unrecognized until symptoms become severe again—often requiring more complex surgery.
Chronic Condition Management
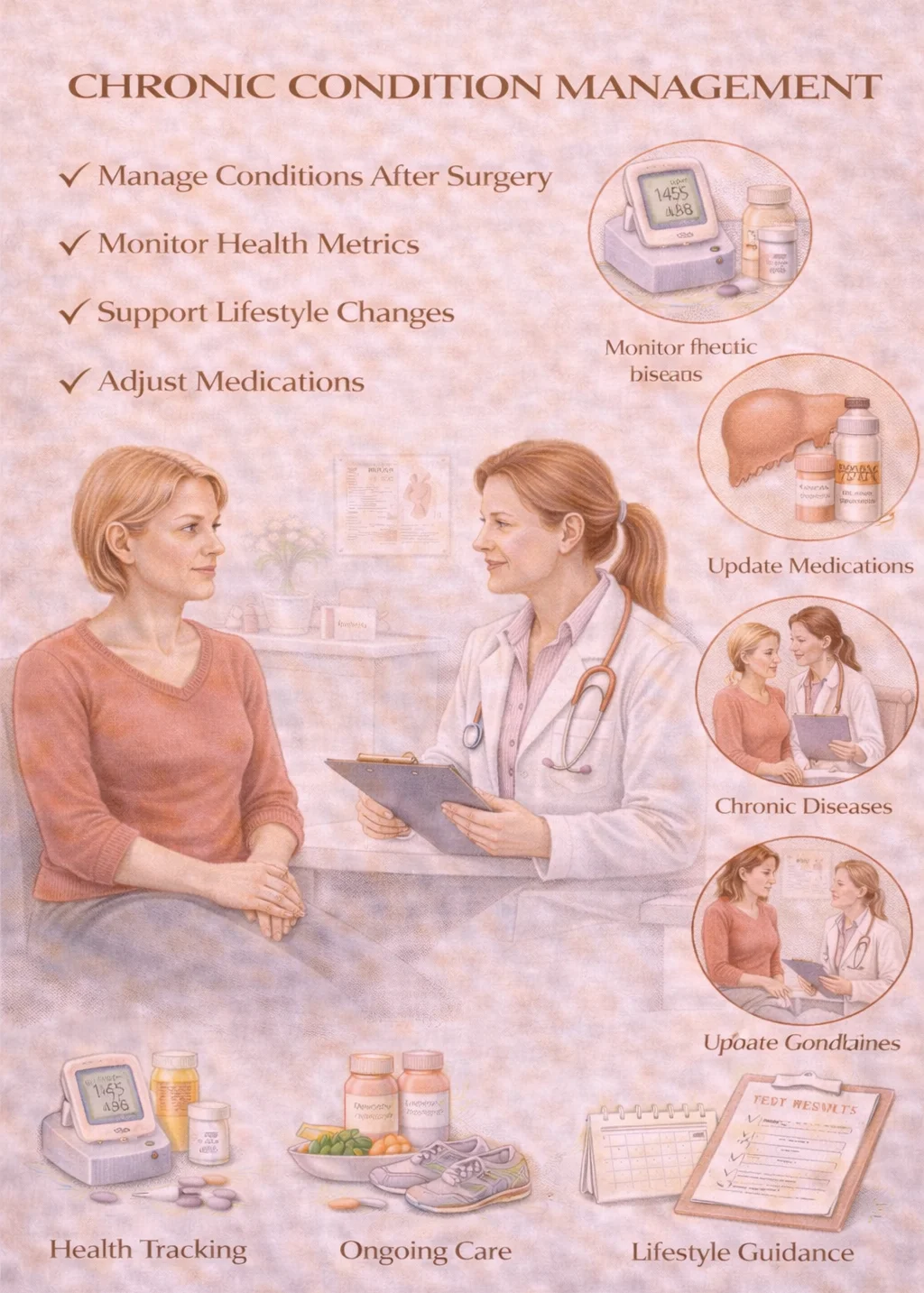
What it is: Ongoing medical care for long-term gynecologic conditions such as endometriosis, PCOS, chronic pelvic pain, recurrent ovarian cysts, menstrual disorders, and hormonal imbalances.
Why it matters: According to the NIH, chronic gynecologic conditions affect millions of women across their lifespan. Long-term management—not one-time treatment—is required for pain control, fertility preservation, metabolic health, and emotional well-being. Care may include hormonal therapy, non-hormonal medical treatment, imaging surveillance, lifestyle and nutrition support, and medication adjustments over time.
When neglected: Without consistent management, women experience disease progression, recurrent emergency visits, worsening fertility outcomes, chronic pain syndromes, and increased mental health burden.
Ongoing Wellness Tracking
What it is: Long-term monitoring of health beyond immediate surgical or medical treatment.
Why it matters: According to the CDC and NIH, women's long-term outcomes improve when providers track weight and metabolism, bone health, hormonal balance, cardiovascular risk, and mental well-being. Preventive tracking reduces late disease detection, avoidable hospitalizations, and long-term disability. Wellness tracking includes routine health screenings, lifestyle optimization, menopause and midlife transition monitoring, bone density surveillance, and ongoing preventive care coordination.
When neglected: Health risks often develop silently for years before symptoms appear—when prevention opportunities have already been missed.
Post-surgical and long-term care are not afterthoughts—they are essential to ensuring that treatment leads to lasting health, recovery, and quality of life.

